“I’m so glad I have a sister. Otherwise, it would just be me, you, Daddy and Suki (our dog).” Those were the words spoken to me recently by my four-year-old daughter, Nika as I rounded the corner from Sasha’s sit to stand recliner and headed towards the hall. I was stunned but tried not to show it. It had been a hard week in the household. I returned from a remarkable caregiver’s workshop in Washington DC to find that Sasha took a swift downturn during my ever so brief absence. We had already taken her to her primary care provider. It was a lengthy visit. As I sat there, the most surreal wave washed over me – a knowledge crest that everything was about to change.
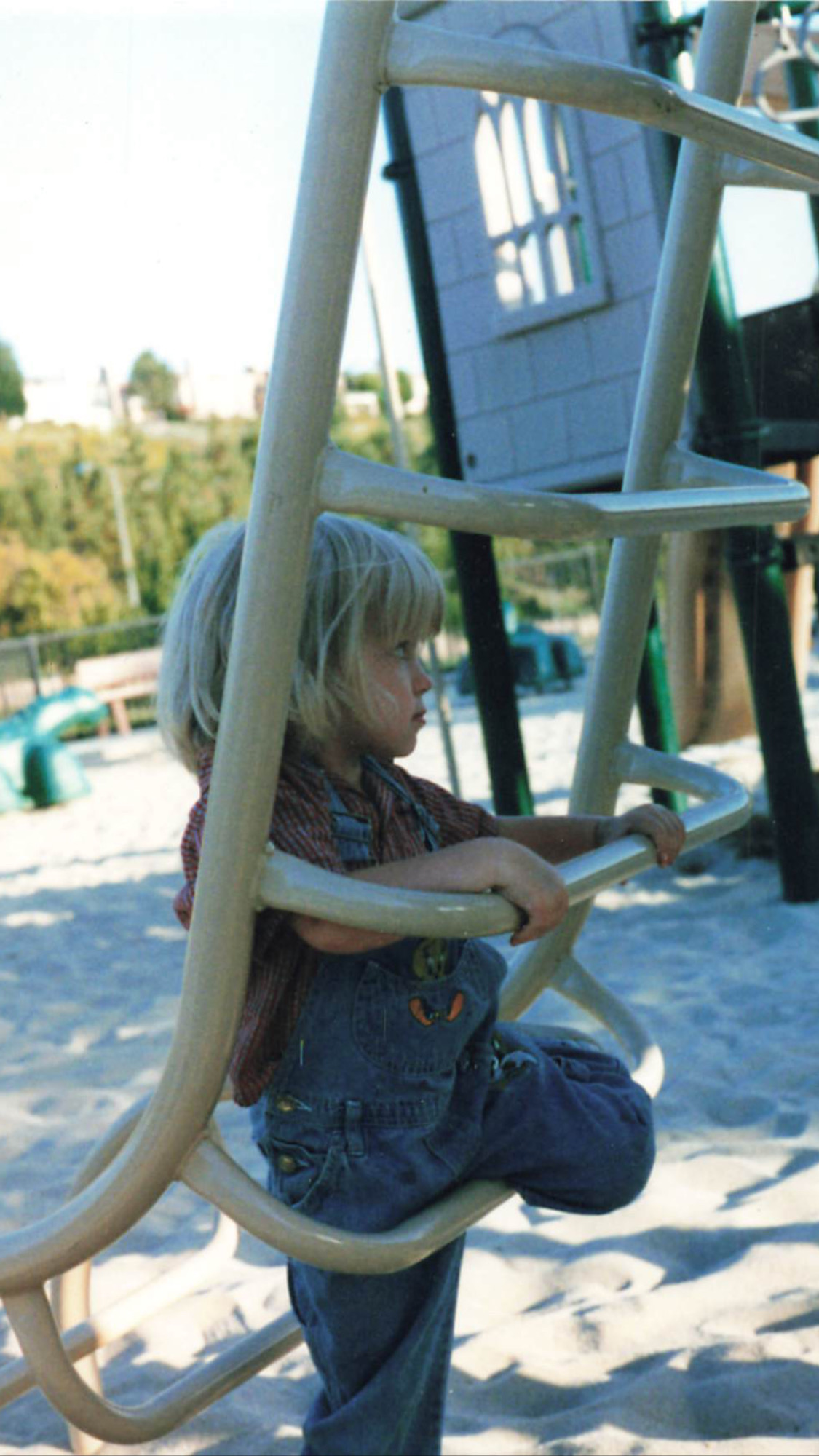
My husband Mike came to the appointment to help get Sasha in and out of our vehicle. We had Nika in tow as the appointment fell on a non-school day. Fortunately, there is a cute park on the clinic’s campus, and the weather cooperated for Nika to play for nearly 2 hours while Sasha and I investigated the next steps in her care plan. I appreciated the levity of Mike sending me time trials as Nika ran laps, “11.77, 12.08, 11.76, 13.31.” Random figures illuminated my phone with no explanation – a pleasant mystery that provided a helpful distraction. The day was a brighter gray than some during a particularly windy October.
appointment fell on a non-school day. Fortunately, there is a cute park on the clinic’s campus, and the weather cooperated for Nika to play for nearly 2 hours while Sasha and I investigated the next steps in her care plan. I appreciated the levity of Mike sending me time trials as Nika ran laps, “11.77, 12.08, 11.76, 13.31.” Random figures illuminated my phone with no explanation – a pleasant mystery that provided a helpful distraction. The day was a brighter gray than some during a particularly windy October.
Daylight savings was coming soon. I sat there silently bemoaning as I waited for Sasha’s PCP to enter the exam room. I’ve always resented the changing of clocks. In my college years, my first taste of adulthood, the time change always took me aback as it collided with an irresponsible modus operandi. Seemingly always in a public establishment, I’d look up only to realize I was an hour off on my given day. Years later, upon having my first child—a daughter with special needs—I would marvel, with frustration, at how deeply her days were affected by adding or taking away even one hour from her already tenuous schedule. Now, in middle age, I resent the changing of clocks for an entirely different reason: who are we to collectively manipulate time? What gives us the societal audacity to control clocks? Do we think we are God? Little did I know—especially in those college years—that time would become such a burden during most of my child-rearing years. I would either wish for it to speed up amid the angst of “When will this ever end?” or to slow down indefinitely so I could cherish the good years.
For nearly two decades, that balancing act came alongside a family unit of 2-3 individuals. While a single Mom to Sasha, there was never a reality of adding a sibling to her chaos. And when I met my second husband as Sasha was approaching age five, I was still a steadfast NO! My hands felt full with an extremely hyperactive child with significant special needs. Being in the throes of destructive sleepless nights, a nocturnal manic state that is common for children with Sanfilippo Syndrome, I knew that adding another child would be the rush of air that pushed down the line of dominos. As Sasha approached nine and we learned of her diagnosis of Sanfilippo Syndrome, we were faced with an unthinkable reality – Sasha’s body carried something fatal. With that realization came the heavy understanding that adding another child would mean they, too, might one day experience a traumatic loss. I doubled down on my steadfast “no” but was that ever the right way to view things? In truth, we could all lose anyone in an instant. Who was I to play God…to try and control any outcome?
My phone continued flashing Nica’s times as I chatted with our PCP’s counterpart, a new nurse practitioner on Sasha’s medical team who was visibly committed to addressing the clinical concerns unfolding. We discussed the preceding week and the cascade of events – Sasha’s sudden struggles with swallowing, her significant weight loss and increased tremors while eating. A swallow study was ordered. I left with numerous instructions, including recommendations for utilizing Sasha’s g-tube for nutrition within a specified framework.
 The g-tube. A gut-wrenching decision that I fought so hard against that preceding year. Nine months of meeting with numerous specialties – Palliative, Genetics, Neurology, Complex Care. Messaging friends and acquaintances in the Sanfilippo community. Reaching out to fellow nurse friends to discuss the clinical implications. Listening to interviews of families before me who navigated the same decision. Middle-of-the-night brainstorming sessions filled with self-reflective thoughts. Looking back on the early days post diagnosis. I remembered sitting in Sasha’s cozy bed, holding her close, telling her I would never initiate any invasive procedure. We would let nature guide us and she could tell me when she was ready to be done with the fight. I told her to never hold on for me or anyone else. When she was tired, she could let us know and we would support her decision to let go. I would never play God.
The g-tube. A gut-wrenching decision that I fought so hard against that preceding year. Nine months of meeting with numerous specialties – Palliative, Genetics, Neurology, Complex Care. Messaging friends and acquaintances in the Sanfilippo community. Reaching out to fellow nurse friends to discuss the clinical implications. Listening to interviews of families before me who navigated the same decision. Middle-of-the-night brainstorming sessions filled with self-reflective thoughts. Looking back on the early days post diagnosis. I remembered sitting in Sasha’s cozy bed, holding her close, telling her I would never initiate any invasive procedure. We would let nature guide us and she could tell me when she was ready to be done with the fight. I told her to never hold on for me or anyone else. When she was tired, she could let us know and we would support her decision to let go. I would never play God.
That time now felt so out of reach, so long ago, like she and I were completely different people. I couldn’t believe the day I found myself sitting in a surgeon’s clinic, waiting for a g-tube consultation. He thought Sasha and I were there to schedule the surgery. In reality, I was there to ask the question, “who are we to think we can change course in an agreed upon pact?”
A highly rushed individual, as trauma surgeons will be, he bound through the exam room door and asked even before making eye contact or sitting down, “What questions do you have for me?” I stared as I waited for him to find his seat and scoot over via his three-wheeled black vinyl stool. A lanky fellow with wisps of black hair along a mostly bald scalp, his shoulders too broad for the wash-faded indigo scrubs, I quietly wondered if he was a long-distance runner. He looked at Sasha and saw my reservations. Knowing we were both rushing to get out of there, I spoke rapidly to squeeze it all in. Eventually, he softened and shared a personal story of his own father temporarily needing a g-tube. He could not impress upon me enough, he stated, the importance of nutrition and hydration in all phases of the lifespan. In that moment, he became more than a surgeon. He became human.
I told him I’d think it over and he shared the process for scheduling. It would not be an immediate phone call, I told him. He encouraged me to call and make an appointment, pointing out that as the day approached, I could always cancel if I was still feeling unsure. He left. I felt a bolstering confidence, ever so briefly. I was not reneging on an agreement made to Sasha so many years ago. And I certainly was not playing God. Was I?
“12.65” Nika’s time trials at the clinic’s park were ending alongside our appointment. Mercifully, Nika did not ask what transpired, an unusual occurrence for her inquisitive nature and foreman mindset overseeing all of Sasha’s care needs. She was consumed in exhilaration by her newfound mastery of time. She had learned through her dad’s coaching that she was slowing down ever so slightly each time she approached the finish line. He had explained that if she made a final push as the imaginary line approached, her time would improve.
There will be times in virtually all our lives, where we will be asked to make a decision standing at the crossroads of faith and uncertainty – at the intersection of medicine and personal philosophy. We may be called to decide for ourselves or for a loved one in a way that directly impacts a clinical outcome.
I have been fortunate to have a care team that welcomes these discussions, even discourse when necessary and who recognizes that philosophy is sometimes malleable and that certainty is never a guarantee. In a world that feels unquantifiable, when making decisions that feel impossible, I came to realize that an 80/20 ratio may be the best that I can do. If 80% confidence in a decision can be obtained, then that is where I will hang my hat. Those decisions may evolve with the revelation of new information or the presentation that is in front of you – our minds can change, and that is alright.
I didn’t know what to say in response that day when Nika proclaimed how happy she was to have a sister. I fought back tears and simply offered, “I’m so glad you have a sister too.”
 Joanne Huff comes to Courageous Parents Network as a long time follower and parent enthusiast of the organization. As the Mother of two girls, the oldest of whom has the rare disease MPS IIIA/Sanfilippo Syndrome, Joanne has benefited tremendously from the intimate parent interviews and candid, vulnerable story sharing throughout numerous thought provoking blog posts. As her daughter’s activities and lifestyle started to slow down with disease progression, CPN became a larger anchor in times of uncertainty and unrest. It is through this lens that Joanne hopes to share experiences and insights via the CPN blog.
Joanne Huff comes to Courageous Parents Network as a long time follower and parent enthusiast of the organization. As the Mother of two girls, the oldest of whom has the rare disease MPS IIIA/Sanfilippo Syndrome, Joanne has benefited tremendously from the intimate parent interviews and candid, vulnerable story sharing throughout numerous thought provoking blog posts. As her daughter’s activities and lifestyle started to slow down with disease progression, CPN became a larger anchor in times of uncertainty and unrest. It is through this lens that Joanne hopes to share experiences and insights via the CPN blog.
Joanne completed nursing school after her daughter’s diagnosis, receiving her Bachelors of Science in Nursing from Plymouth State University, Plymouth NH. She enjoyed community liaison work with home care providers of adults with special needs up until her own daughter’s care became increasingly more involved. In addition to serving on the Boards of New England Regional Genetics Group (NERGG) and Adaptive Sports Partners through 2024, she has found great purpose in volunteer work advocating for policy improvements and change in Washington DC with the National MPS Society. In her free time, Joanne seeks balance and refuge with yoga, hiking and performing as an ensemble Soprano vocalist with the Pemigewasset Choral Society. When not blogging for CPN, Joanne enjoys sharing offerings on her personal Blog Folding Origami for God. She resides in Bow New Hampshire with her two daughters, Sasha and Nika, her husband Mike and her yellow lab Suki.